What is already known about the topic?
Treatment for Dupuytren's contractures is mainly symptomatic, with fasciectomy being the reference surgical approach. As a new therapeutic alternative, collagenase injections are presently being proposed, although this new treatment option must still be validated by means of controlled trials.
What does this article bring up for us?
Our study findings allow us to better define, within the therapeutic arsenal available to date, the role of collagenase injections for MCP involvement in Dupuytren's disease. This novel treatment option is easy to use and quick in action, and can thus be applied at consultation.
INTRODUCTION
Dupuytren’s contracture (DC) is a connective tissue disorder caused by an excessive production of collagen in the palmar fascia. Advances in research over the last few decades have allowed for a better understanding of the cellular and molecular mechanisms that drive a healthy fascia to become a pathological fibrous tissue (1).
The process is progressive and begins with a proliferative phase during which fibroblasts transform into myofibroblasts. This phase is followed by the involution phase during which the myofibroblasts line up along tension lines. Finally, in the residual phase, myofibroblasts disappear, leaving thick bands of collagen. These different phases lead to the formation of nodules and contracted fibrous bands. As a result, irreducible flexion contractures occur at finger joints, with varying functional deficits that can sometimes be a severe handicap.
The prevalence of DC is estimated between 0.6 % and 31.6 % in Western countries (2). Its etiology is still uncertain. A genetic origin was considered base on research showing family cases and cases among twins, with an increased incidence of DC in Scandinavian countries (3). Factors contributing to the development of DC include the following: family history, age, weight or low BMI, diabetes, alcoholism, or repetitive strain injuries. The prevalence of Dupuytren’s contracture is greater in men (2% of men after 40 years of age (8 to 9 men to 1 woman) and the age of disease onset is earlier in men (3). Evolution is slower in women (3), which explains why more men than women resort to therapy.
Treatment for DC remains symptomatic, as no cure currently exists. Therapeutic options are surgical fasciectomy or percutaneous needle fasciotomy. Choice of therapy depends on severity of the disease, patient age, comorbidities, the need for post-operative monitoring, or patient preferences (4). Open fasciectomy remains the most common technique. Regardless of the chosen treatment modality, recurrence is very common given the progressively developing nature of Dupuytren’s contracture. Numbers vary depending on the studies but frequency of recurrence after treatment is high in all cases.
Collagenase as a therapeutic alternative to surgery in Dupuytren’s contracture seems like a promising option (1). Interest in this technique is growing, and the scientific literature has expanded (1,6). It was first approved in the USA by the Food and Drug Administration in 2010, and then in Europe by the European Medicines Agency. It arrived in Belgium in 2012 under the trade name Xiapex®.
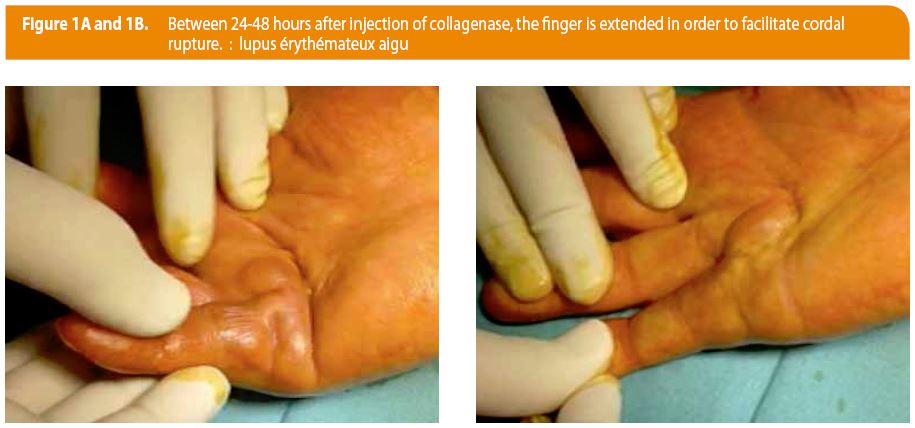
The therapeutic principle of Xiapex® is based on an enzymatic process that associates two bacterial collagenases, AUX-I and AUX-II, isolated and purified from the anaerobic fermentation of the Clostridium Histolyticum strain. Administration of Xiapex® involves a single injection of the collagenase in a palpable pathological cord. Between 24-48 hours after injection, the finger is extended in order to facilitate cordal rupture (Figure 1A-B). Treatment effectiveness is evaluated by measuring the loss of extension with the help of a goniometer. A residual flexion of < 5° indicates treatment effectiveness.
The aim of this pilot study was to evaluate the use of collagenase as a new therapeutic technique in Dupuytren’s contracture, and to compare it to fasciectomy, whose effectiveness is already well-established. Treatment impact was evaluated after one year on pain, daily activity and satisfaction to assess whether its introduction in the existing therapeutic landscape is justified.
MATERIAL/PATIENTS
We compared 19 patients who benefited from a collagenase injection (the Xiapex group) to 19 patients who benefited from the traditional open fasciectomy (the surgical group). All patients were treated by the same operator. The two groups were compared pre-treatment and post-treatment, both immediately following the procedure and at 12 months. The study was approved by the local ethics committee (N° B40321523492) and the protocol conformed to the ethical guidelines of the 1975 Declaration of Helsinki. Our study is registered in clinical trial.gov PRS number NCT02355301.
The Xiapex group was made up of 17 men and 2 women with a mean age of 64 years (SD 8). No patient had previously received another type of treatment for Dupuytren’s contracture. Fifteen patients benefited from a metacarpohalangeal (MCP) injection; the remaining four received proximal interphalangeal (PIP) injections. Injections took place at D5 for eight patients, D4 for seven patients, D3 for one patient and D2 for the last patient. Two patients had both D4 and D5 damage. Only one of the two digits was treated by injection.
The surgical group also consisted in 19 patients, made up of 15 men and 4 women. Mean age was 60.4 years (SD 12). Twelve MCPs and sixteen PIPs were treated. Multiple cords or multiple digits were therefore treated in the same patient in the same surgical time.
METHODS
We first conducted student’s t-tests to verify homogeneity between groups (Xiapex and surgical) who benefited from an intervention at either the MCP or the PIP joint. That is, we examined whether groups were equal in terms of age and pre-treatment joint mobility in extension (variables were expressed in terms of loss of extension). Subsequently, we evaluated whether the different treatments resulted greater or less joint mobility by comparing loss of extension results both pre- and post-treatment (immediate post-treatment and at 12 months). We performed a two-way repeated measures ANOVA (time x treatment). The p-value of the interaction was interpreted. For each analysis, normality of distribution and equal variances were tested with the Shapiro-Wilk test. Variables are expressed as means with standard deviation.
Finally, we examined whether the two treatments differed in terms of pain (via the Visual Analogue Scale, or VAS score), daily life activities (via the Disabilities of the Arm, Shoulder and Hand, or DASH score), and satisfaction (via a scale ranging from 0 to 5). Data were recorded during the post-treatment period at 12 months. We conducted a rank sum tests for this data as distribution normality and equality of variances were not respected. In addition, given certain scores were expressed as ordinal data (satisfaction), we expressed results as medians and interquartile ranges. Significance level was set at 0.05.
RESULTS
Loss of extension between the Xiapex group and the surgical group, pre- and post-treatment
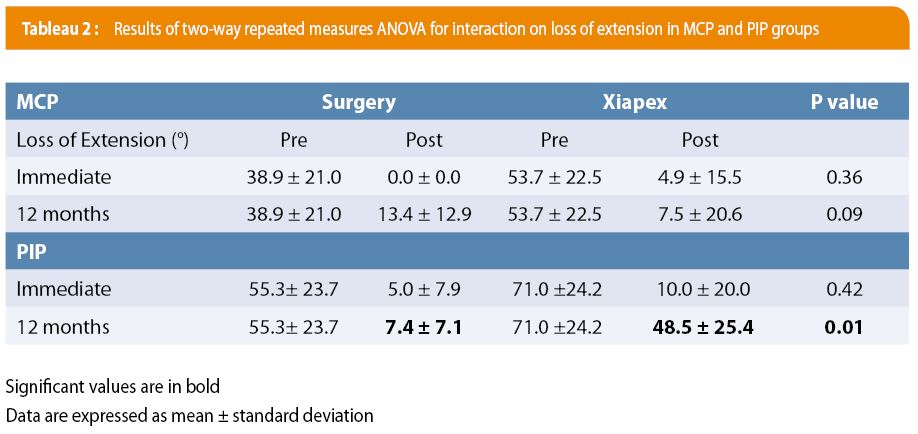
We first checked to see that both groups were homogenous pre-treatment. No significant differences were observed between the two cohorts (see Table 1). Regarding loss of extension immediate post-treatment for the MCP group (see Table 2), residual loss of extension was measured at 0.0° (± 0.0) in operated patients, versus 4.9° (± 15.5) for injected patients (p = 0.36). At 12 months post-treatment, residual extension was 13.4° (± 12.9) in operated patients, versus 7.5° (± 20.6) in injected patients (p = 0.09). Therefore, no significant difference was found between the two groups, both in the immediate post-treatment period and at 12 months.
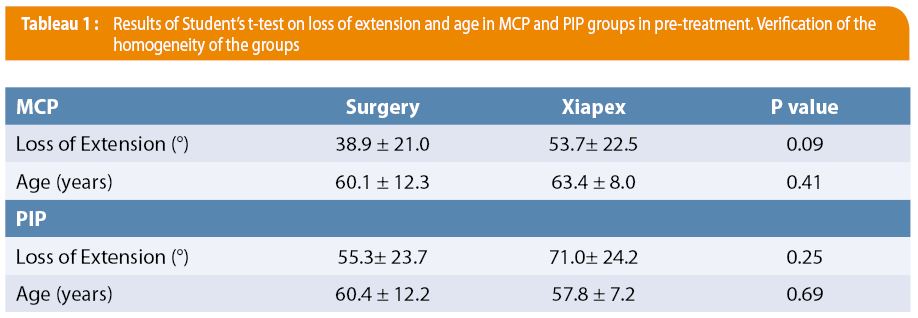
As for loss of extension immediate post-treatment for the PIP group (see Table 2), residual loss of extension was measured at 5.0° (± 7.9) in operated patients versus 10.0° (± 20.0) for injected patients (p = 0.42). A 12 months post-treatment, residual loss of extension was 7.4° (± 7.1) in operated patients, versus 48.5° (±25.4) in injected patients (p = 0.01). A non-significant difference was therefore observed between these two techniques in the immediate post-treatment period, while a significant difference was observed at 12 months post-treatment, with less extension deficit in the surgical group (p < 0.05).
Subjective data between the Xiapex group and the surgical group, post-treatment
Concerning subjective data in patients with MCP damage (see Table 3), the VAS scale showed a median score of 3 out of 10 [0.75-5.0] for operated patients and 0 out of 10 [0.0-2.0] for patients having received an injection. This difference was significantly different (p = 0.02), with less pain in the Xiapex group. The DASH score was also significantly lower in the Xiapex group (2.3 0.0-14.7]) compared to the operated group (18.2 [9.4-38.2]), p = 0.02. Lastly, patient satisfaction, evaluated on a scale of 0 to 5, was significantly higher (p = 0.0004) in Xiapex patients (5 out of 5 [4.0-5.0]), compared to the operated group (2 out of 5 1.0-4.0]).
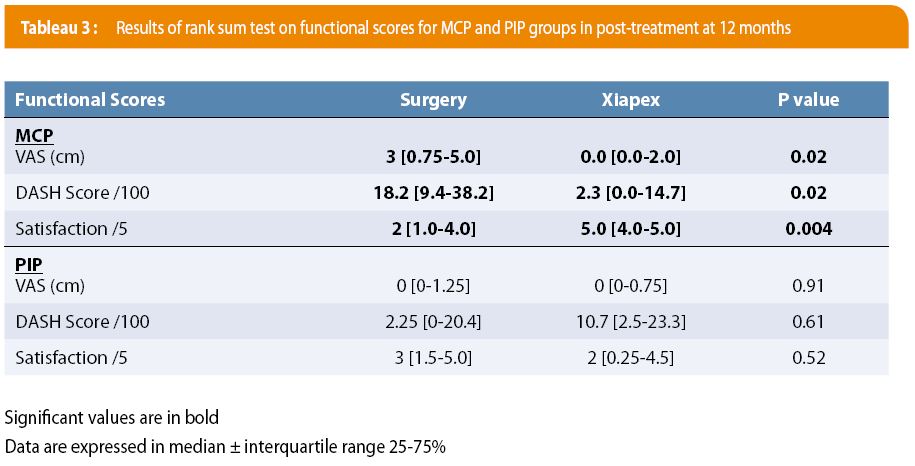
Finally, regarding subjective data in patients with PIP damage (see Table 3), the VAS scale showed a median score of 0 out of 10 [0.0-1.25] for operated patients and 0 out of 10 [0-0.75] for Xiapex patients. This difference was not significantly different (p = 0.91); no significant difference was therefore observed between the two techniques in terms of pain for the PIP joint. The DASH score was 2.24 [0-20.4] for operated patients and 10.7 [2.5-23.3] for Xiapex patients, which was also non-significant (p = 0.61). Patient satisfaction was 3 out of 5 [1.5-5.0] for operated patients versus 2 out of 5 for the injected group [0.25-4.5], with no significant difference between these two groups (p = 0.52).
DISCUSSION
From this pilot study, our results show that collagenase injection is an effective treatment with which patients are satisfied and that has few major side-effects. It is important, however, to distinguish results at the MCP joint, which showed very favorable results, and the PIP joint, for which the gain in extension and patient satisfaction were less favorable. PIPs are generally more susceptible to joint stiffness, which could explain this difference.
Comparison with the literature: Collagenase, surgery and needle fasciotomy
Our results are encouraging and are consistent with other studies. The CORDLESS study (6) is a retrospective, multicenter study based on the follow-up at 2, 3, 4, and 5 years of patients who received a collagenase injection in various clinical studies. A loss of extension < 5° after injection was defined a successful treatment. Recurrence was defined as a contracture > 20° with a palpable cord, or a case requiring a secondary medical intervention or surgery to correct the new contracture or its aggravation. Results after 5 years have just been published, with a cohort of 644 patients for a total of 1081 treated digits. 623 digits were successfully treated. At 5 years, 47 % (291/623 digits) showed recurrence: 39% (178/451) of MCPs and 66 % (113/172) of PIPs. Of the cases that showed recurrence, 53 % of patients underwent additional treatment (fasciectomy, additional injection, or other). Only one complication attributable to the collagenase injection was observed (cutaneous atrophy at the injection site). The results of this study confirm that recurrence rates of collagenase injections are comparable to recurrence rates of surgical interventions published in the literature5. CORDLESS study concludes that effectiveness is comparable between the two treatments for MCP. It also highlights the less favorable results of collagenase injections at the PIP level.
When comparing to surgery, for patients with MCP damage, our results show that collagenase injections are just as effective in terms of increased extension, both in the immediate post-treatment period and at 12 months. Moreover, in terms of pain, functionality and patient satisfaction, the injection method showed favorable results. This could be explained by the fact that the intervention is generally less cumbersome for the patient. For patients with PIP damage, both treatments are equally effective during the immediate post-treatment period, but at 12 months, there is a sharp decline in extension increase, indicating the high recurrence rate of collagenase injections within this group (75%). This recurrence rate most likely had a negative effect on functionality and patient satisfaction for the injected group. Nonetheless, pain scores were identical for both groups.
These results lead us to conclude that collagenase injections are an appropriate alternative to surgery when treating Dupuytren’s contracture at the MCP level. Results are much less encouraging at the PIP level, as previously described (6). Collagenase injections are advantageous in terms of ease of use, reproducibility, and its simple post-intervention procedures. Although it was not the case in our study, injections can be carried out during consultations, under local anesthesia, without hospitalization. In most cases, no monitoring of wound or dressing needs to be organized. However, with some patients, it is necessary to remain cautious and to establish a regular monitoring of the wounds. Some studies even claim there is limited need for physical therapy and splints (5).
Collagenase injections are often compared to needle fasciotomy. This technique is uncommon in Belgium. Mostly used in France, it has a long term recurrence rate that ranges from 60 to 85 %. Both procedures are simple, reproducible and easily manageable for the patient. While they are considered competing options, studies comparing collagenase injections to needle fasciotomy are scant.
Comparing treatment options in terms of financial cost
As both treatments appear to have similar results with regards to effectiveness, it is important to evaluate the differences in terms of cost. Some studies have considered the budget impact of these two procedures. An American study (7) was conducted to compare cost-effectiveness between needle fasciotomy, fasciectomy and collagenase injections. Collagenase injections are financially advantageous when the price is less than $945, given the recurrence rates previously reported in clinical results. If recurrence rates were to increase, collagenase injections would lose their financial value compared to needle fasciotomy.
In addition, a Spanish study (8) looked at the financial impact of collagenase injections compared to surgery, this time accounting for all costs relative to the overall care of the patient for both techniques (consultation, administration, hospitalization, post-procedure care, medications and rehabilitation). Average cost of collagenase injections was €1220 (including four consultations and 1.5 bottles for each treated digit), with a minimum of €898 (1.1 bottles/digit, and 3 visits). Average cost of fasciectomy was €2250 (€1703 for outpatient care and €2467 with hospitalization). The cumulative study over 3 years showed that budget impact was significantly less for collagenase injections. Let us note a potential conflict of interest by the authors considering sponsorship by a pharmaceutical company.
In Belgium, the amount charged to the patient for the product is €25. Health insurance covers €700. In order to obtain reimbursement, the surgeon measure with goniometer a retraction in flessum of 20° on one joint. Only two joints can be damaged per hand. A clinical report and a photograph must be included in the file. A maximum of 3 injections are reimbursed by hand every year with a cumulative maximum of 8 bottles by hand reached over the years. Injections must be performed by an orthopedic surgeon or a plastic surgeon experienced in treating Dupuytren’s contracture, with specific training in Xiapex injections (9).
Comparing treatments in terms of complications
In terms of complications, when monitoring our patients, we observed minimal complications, namely self-limiting local edema and/or bruising. The extension maneuver of the finger, performed after 24-48 hours, caused a skin tear in four cases (21 %, see Figure 1A-B & 2). One case of algodystrophy was reported. No tendon ruptures were reported.

The literature has shown that in terms of risk, collagenase injections are top ranking (see Table 4) given their minor complications and short recovery time. Open fasciectomy has complications linked inherently to surgery and wound, such as nerve damage, infection, stiffness and a longer recovery time. Tendon rupture, nerve damage and bruising are also potential complications linked to needle fasciotomy. Nonetheless, needle fasciotomy remains a simple, reproducible and inexpensive technique that can be conducted on several digits simultaneously.

Limits
The results of this pilot study should be confirmed on a larger cohort of subjects especially concerning PIP patients. Moreover, the loss of extension is most important (but not significant) for Xiapex goup. Most affected patients should be integrated at the outset in the surgery group. In addition, it would be interesting to evaluate the functional effect of treatment pre and post processing.
CONCLUSION
The collected data helped attain the goal of this study, which was to position the use of collagenase injections within the landscape of existing therapies for Dupuytren’s contracture.
Collagenase injections show a similar effectiveness to the surgical alternative when treating symptomatic cords at the MCP joint. For the PIP joint, results were less promising but the collagenase injections remain quite acceptable with a noticeable improvement. This treatment is an alternative to consider compared with surgery, especially if wearing removable brace is prescribed for a long period after the injection to keep the result obtained after the finger stretch.
Collagenase injection may nevertheless be suggested to PIP patients with comorbidity. The technique is simple, minimally invasive, and is less cumbersome for the patient. It allows fast recovery and does not require wound monitoring. As such, collagenase injections seem to be a realistic alternative to open surgery.
Current literature on collagenase injections is flourishing, which will allow for more and more long-term data with regards to recurrence rates, thus increasing the procedures’ reliability, which may subsequently broaden its use. The budget component remains to be explored in order to determine the optimal treatment in terms of cost-effectiveness, especially when accounting for the inevitable recurrences within each treatment option.
RECOMMENDATIONS PRATIQUES
Les injections de collagénase montrent de bons résultats similaires à la chirurgie mais principalement pour les articulations métacarpo-phalangiennes. Cette technique est facile, peu invasive, rapide et peut se faire en consultation. Elle est trop peu utilisée dans notre pays.
AFFILIATIONS
a Grand Hôpital de Charleroi, Department of Orthopedics, Grand Rue 3, 6000 Charleroi, Belgium. Email : Email fernand.van.innis@skynet.be; serge.troussel@gmail.com and Tleq@hotmail.com ;
b Cliniques universitaires Saint-Luc, Department of Orthopedics and Traumatology, Avenue Hippocrate 10, 1200 Brussels, Belgium. Email : alexandre.hupez@student.uclouvain.be; Xavier.Libouton@uclouvain.be
c Université catholique de Louvain, Institut de Recherche Expérimentale et Clinique IREC, Pôle Computer Assisted Robotic Sugery pole CARS, avenue Mounier 53, B15307, 1200 Brussels, Belgium. Email : christine.detrembleur@uclouvain.be
CORRESPONDANCE
Pr Christine Detrembleur
Université catholique de Louvain, Institut de Recherche Expérimentale et Clinique IREC,
Pôle Computer Assisted Robotic Sugery pole CARS,
avenue Mounier 53, B15307, 1200 Brussels, Belgium.
Email : christine.detrembleur@uclouvain.be
REFERENCES
1. Hentz VR. Collagenase injections for treatment of Dupuytren disease. Hand Clin 2014; 30(1):25-32.
Ouvrir dans PubMed
2. Lanting R, Broekstra DC, Werker PM, van den Heuvel ER. A systematic review and meta-analysis on the prevalence of Dupuytren disease in the general population of Western countries. Plast Reconstr Surg 2014;133:593-603.
Ouvrir dans PubMed
3. Pajardi G. Dupuytren’s disease. Fessh International Course 2015;82-170.
4. Denkler K. Surgical complications associated with fasciectomy for Dupuytren’s disease: a 20-year review of the English litterature. Eplasty 2010;10:116- 33.
Ouvrir dans PubMed
5. Hurst LC Badalamente MA, Hentz VR, Hotchkiss RN, Kaplan FT, Meals RA, Smith TM, Rodzvilla J; CORD I Study Group.Injectable collagenase clostridium histolyticum for Dupuytren’s contracture. N Engl J Med. 2009;361(10):968-79.
Ouvrir dans PubMed
6. Peimer CA, Blazar P, Coleman S, Kaplan FT, Smith T, Lindau T. Dupuytren Contracture Recurrence Following Treatment With Collagenase Clostridium Histolyticum (CORDLESS [Collagenase Option for Reduction of Dupuytren Long-Term Evaluation of Safety Study]): 5-Year Data. J Hand Surg Am 2015;40(8):1597-605.
Ouvrir dans PubMed
7. Chen NC, Shauver MJ, Chung KC. Cost-effectiveness of open partial fasciectomy, needle fasciotomy, and collagenase injection for Dupuytren contracture. J Hand Surg Am 2011;36:1826–34.
Ouvrir dans PubMed
8. De Salas-Cansado M, Cuadros M, Del Cerro M, Arandes JM. Budget impact analysis in Spanish patients with Dupuytren’s contracture: Fasciectomy vs. collagenase Clostridium histolyticum. Chirurgie de la main 2013;32:68–73.
Ouvrir dans PubMed
9. Warwick D. Dupuytren’s Disease. FESSH Instructional Course 2015. Edizioni Medico Scientifiche, 2015.
10. Warwick D. Final Thoughts. In: Giorgio Pajardi. Dupuytren’s disease. FESSH International Course 2015. Edizioni Medico Scientifiche. 2015, p. 238.