BACKGROUND
The starting point of the patient’s history is a relatively frequent disease: diverticulitis(1). Most of them are uncomplicated and treated by conservative treatment. In our case the combination of these two different entities led to an extremely rare and life-threatening consequence. Even taken separately, pylephlebitis and HITT syndrome are rare. After reviewing the literature with “pylephlebitis” and “bowel ischemia” as search terms in Pubmed, we only found two articles where ischemia led to a bowel resection (2,3). When looking for “heparin-induced thrombocytopenia” and “bowel resection” we found one single case(4). Searched together, those entities show no result. This case report is an opportunity to discuss two rare conditions leading to a significant bowel resection.
CASE HISTORY
We present the case of 31-year-old-man who has been admitted at the emergency room with abdominal pain and gastro-intestinal complaints. At this time, the clinical examination was unspecific. The blood sample was within the normal values. The patient’s past medical history was significant for obesity (BMI 36 kg/m²). The familial history has contributed for a factor II G20210A mutation of his father. Injected computed tomography (CT) showed a thickening of the sigmoid wall with infiltration of the surrounding fat and hypodensity of the portal and superior mesenteric veins with no sign of hepatic or small intestine hypovascularization (Figures 1 and 2).


The blood analysis showed no coagulopathy or hepatic tests disturbancies. The patient was hospitalised and treated with broad-spectrum antibiotics and low weight molecular heparin (LWMH) at therapeutic doses. Three days later, because of hyperthermia and chills, a new CT scan was performed and depicted a thrombus extension in the splenic vein and in the right and left intrahepatic veins (Figures 3 and 4).


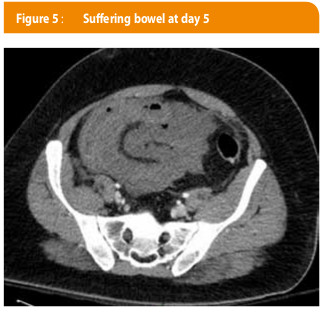
The patient was consequently transferred to intensive care unit of the Cliniques universitaires Saint-Luc. The antibiotics were maintained, but the LWMH was switched to continuous infusion of unfractionated heparin (UFH). On day 5, the patient presented an acute abdominal pain and a worsening of his vital parameters, imposing a new imagery by CT scan which revealed an aggravation of the prior lesions as well as suffering signs of the jejuno-ileum. The laboratory results showed lactic acidosis, white blood count at 20 000/mm³, LDH at 279 UI/L (<250 UI/L), no hepatic perturbations, a drop of the thrombocytes count from 258 000/mm³ to 43 000/mm³ (normal value >150 000/mm³) and a perturbation of the haemostasis parameters. The UFH was switched to danaparoid since a HITT was suspected. This diagnosis was confirmed with the presence of anti-PF4 antibodies at a level of 3.6 U/mL (normal <1U/ml). All the bacteriological tests remained negative. The patient engaged in a distributive shock and was taken to the operative room. During the laparotomy, necrosis of the jejuno-ileum was observed. The patient underwent a resection of over 2 meters of small bowel, an ileostomy at 20 cm from the Treitz’s angle and a mucous fistula at 70 cm from the ileocaecal valve were made (Figures 5 and 6). Post-operative course was uneventful. Total parenteral nutrition was started as the patient suffered from small bowel syndrome. Parenteral nutrition has to be continued at home, but the patient was allowed to have oral nutrition for quality of life reasons. Anticoagulation was continued with Acenocoumarol, a vitamin K antagonist with a targeted international normalized ratio between 2 and 3. To complete the evaluation of this massive venous occlusion a molecular analysis was performed and confirmed a heterozygous G20210A mutation of the factor II (prothrombin). Ileostomy closure will be considered in the next months.

DISCUSSION
Pylephlebitis
Introduction
It is important to define the term pylephlebitis to limit our review of the literature because there are different conditions which can lead to a portal vein thrombosis (PVT)(5). We define pylephlebitis as a suppurative PVT or one of its tributaries and it has to be a complication of an intra-abdominal infection or inflammation. It is a rare complication and the incidence is unknown, as experience is only limited to case reports. One could extrapolate the incidence of pylephlebitis based on the incidence of mesenteric venous thrombosis which reaches 2,7/100000 person-years (5). Even though Kanellopoulou et al. describe a decreasing mortality rate since 1985 (6), probably due to imagery and treatment improvements, mortality remains high: 11% in a review of 95 cases (7). The physiopathology remains unclear. Some authors describe a possible mechanism based on the induction of platelet thrombi by bacteria and antibodies (8). Another area of research is described in a case report where bacteria were related to the development of transient anti-cardiolipin antibodies (9), but more studies are needed. The process starts usually in the small mesenteric veins that drain the infected area, spreads to the portal venous system and hematogenously to the liver, giving complications related to the sites involved.
Clinical presentation
The presentation of pylephlebitis is non-specific. Symptoms such as fever, abdominal pain, vomiting or diarrhoea are usually noticed. Jaundice can be observed in advanced stages and is due to hepatic involvement. Bloody stool, peritonitis or bloody ascites may be signs of bowel necrosis. In our case none of those advanced signs were found but the patient presented a distributive shock due to his bowel infarction. The laboratory tests are unspecific as well. Leucocytosis associated with increasing C-reactive protein are the most common findings (6). A part from the difficulty to manage this condition may probably be attributed to the non-specific presentation. In a case, reported by Fukahori et al., pylephlebitis was discovered 40 days after the patient was admitted for isolated fever without any inflammatory syndrome or leucocytosis, illustrating the difficult challenge of an early diagnosis (10).
Aetiology
Prior to the modern antibiotic’s era, appendicitis was the most frequent condition causing pylephlebitis, but with the improvement of the medical and surgical treatments, such complications dramatically decreased over time. Nowadays, the majority of pylephlebitis present an underlying diverticulitis, with 1/3 of the patient in a review of 100 cases. In the latter series, appendicitis, inflammatory bowel disease and pancreatitis were the next most common causes. Beside the infectious disease, our patient also has a familial history of factor II G20210A mutation. This is an inherited mutation leading to an overexpression of the genes coding for prothrombin, which is a procoagulant factor (Table 1).

We tried to evaluate if thrombophilic inherited disorders were often related to pylephlebitis. In this 100 patient review, only 1/3 where screened for inherited thrombophilia and 1/3 of those presented an abnormality (6). We found a review of 92 patients with portal venous thrombosis (non exclusively suppuratives ones) that reported an increased relative risk for patients with inherited thrombophilic disorders (11). Our patient presented thus a relative risk of 1.4, according to this review (11). Note also that an article on 10 patients showed that the frequency of G20210A factor II mutation was higher in patients with idiopathic portal vein thrombosis, giving a clue to understand the implication of this pathology in our case (12). In the literature, we found a similar situation. A patient, with a pylephlebitis developed after a foodborne illness, evolved to a bowel necrosis leading to a surgical resection. A thrombophilic screening has been made and it showed that the patient had this factor II mutation (2).
Diagnosis
Early diagnosis of pylephlebitis is challenging. Short of the possibility to have a direct blood culture of the portal flow, the diagnosis has to be made with other clinical signs. The enhanced CT scan is the most used tool to assess the underlying condition and the thrombosis at the same time. CT scan is preferred to MRI for practical reason. Portal venous phase imaging is the best diagnostic modality because it can detect the thrombi and can depict hepatic abscesses or bowel ischaemia if present (7). Ultra-sonography is especially indicated to assess the portal flow. Blood cultures are systematically performed but there are only positive in 44% (7).
Outcomes
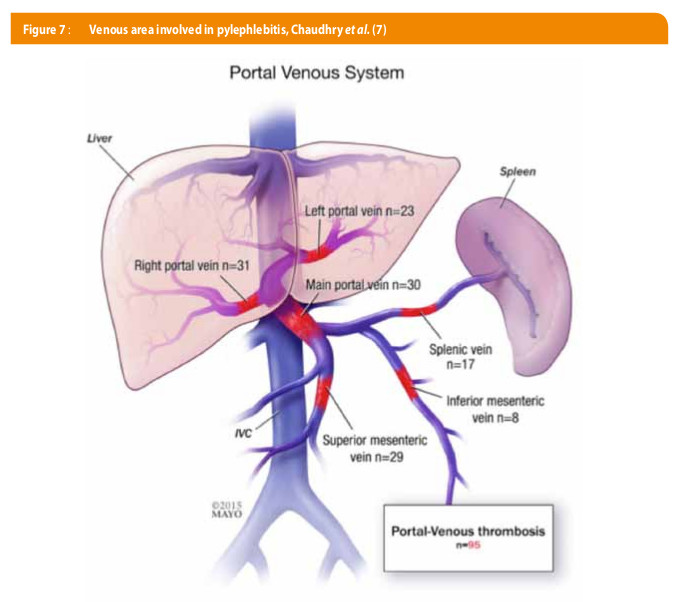
The thrombus may extend to the tributaries of the portal vein. The most common site of thrombosis is the portal vein (including intrahepatic portal veins), the first extension is in the superior mesenteric vein, followed by splenic vein and then inferior mesenteric vein (7). The sites of extension may define the types of complications. Figures about the total complications of pylephlebitis where found in two articles (6, 7) and were mostly inconsistent (6, 7). In the most recent one, amongst 95 patients, only a fifth, presented complications, 12 % presented chronic thrombosis, 4% bowel ischemia (only 1 underwent surgical resection), 2 % hepatic abscesses and only one presented splenic infarction. This paper published a recovery rate of 89 % with a mortality of 11% (7), versus 22% (6) or 32% (13) in older reviews. The origin of the infection does not play a role in the disease severity (7). The severity of the outcome is probably more related to the patient’s co-morbidity. This kind of thrombosis of the portal vein rarely lead to portal hypertension or organ ischaemia, forcing the observation that most of pylephlebitis are non-totally occlusive. In our case, there was still a portal flow but no mesenteric flow anymore. This total mesenteric occlusion is rare enough in the literature to incite us to make further investigations.
Treatment
In absence of robust studies on this condition, there are no consensus or guidelines in management. The care recommendations are only based on case reports. However, it is widely accepted to start an early treatment with a broad-spectrum antibiotic covering enteric gram-negative Bacilli, anaerobic and aerobic Streptococcus (13). This therapy must be used even in the absence of positive bacteraemia (6, 7, 14), and must be adapted according to the cultures. Concerning the treatment duration, Plemmons et al. argue for 4 to 6 weeks of antibiotic therapy to prevent hepatic abscesses, and 6 weeks if abscesses are present (13). The role of anticoagulation is much more debatable. In most of the reviews, anticoagulant therapy is prescribed and shows a lower mortality rate than without treatment (6, 7, 13, 14). Kanellopoulou et al. advocate that with an early anticoagulation treatment an improved outcome is observed with a higher recanalization rate, lower mortality and lower rate of portal hypertension (6). There is no data in the literature as for what type of anticoagulant should be used. The duration of the treatment is even more controversial. Recommendations are made for venous porto-mesenteric thrombosis and advocate to treat it like a postoperative complication and to evaluate if there are thrombophilic mutations in which case the patient has to be treated longer and followed by a haematologist (14,15). Of course, the risks of anticoagulation have to be balanced with the benefits. In this case, the patient was straightaway treated with antibiotics and heparin because of the large extension at the first imaging, but the heparin had to be switched to danaparoid because the patient developed a heparin induced syndrome probably responsible for the extension of the lesions (Table 2) (Figure 7).

HEPARIN-INDUCED THROMBOCYTOPENIA (HIT)
Such an extension of the thrombus in pylephlebitis is uncommon and was associated with the presence of a heparin-induced thrombocytopenia and thrombophilia.
There are two types of HIT. Type 1 is the most frequent. It typically manifests within the two first days after heparin initiation. It is characterized by a transient decrease in platelet count normalizing despite continuing heparin. It is probably due to transitory platelet’s activation. This syndrome is clinically insignificant and does not require interruption of heparin. Type 2, also known as heparin-induced thrombocytopenia and thrombophilia, is rare and more serious. This syndrome is an immune-mediated disorder. The physiopathology is complex. To summarize, during the platelet’s activation the platelet factor 4 (PFA-4) is released. When combined with heparin, this complex can form an antigen recognized by specific antibodies. This PFA-4/heparin-antibodies complex can bound to platelet’s surface and lead to additional platelet activation, amplifying the coagulation process. This reaction is sustaining the production of thrombin and is associated with a paradoxal thrombophilic status associated with thrombocytopenia (16). Regarding the pathophysiology, Krauel K et al. showed that PFA-4 can bind lipopolysaccharides to gram negative bacteria resulting in a complex resembling those on PFA-4/heparin suggesting that bacteria could participate in the suppurative thrombosis we described in this case (17).
The HITT is defined by a drop in the platelet count of 50% from the highest figure after the initiation of heparin or the occurrence of a new thrombosis after the beginning of the treatment, associated with the detections of anti PFA-4/heparin antibodies. It’s incidence is around 1/5000 hospitalized patients but with a large variability among general population(16).
Thrombocytopenia occurs in 85 to 90% of the patients (18). However, it is important to remember that HITT can also occur without thrombocytopenia and that 25 % of patients develop thrombosis before thrombocytopenia (18). The platelet drop typically occurs between 5 to 10 days after starting the heparin and rarely decrease below 20 000/mm³, making spontaneous bleeding rare (19) (Table 3). Thrombosis is the most frequent complication of untreated HITT. Its presentation is mostly on venous territory with mainly distal venous thrombosis and/or pulmonary embolism with 17% to 55% of untreated patients (18). Arterial events such as limb artery thrombosis, stroke or myocardial infraction are much more rare (3% to 10%)(18). There are many manifestations such as limb gangrenes, adrenal haemorrhagic necrosis due to adrenal vein thrombosis, disseminated intravascular coagulation, and there is an interesting case report related to our subject, which describe mesenteric and coeliac occlusions following HIT after a major vascular surgery (3, 4). Due to the prior pylephlebitis, the presentation of our patient is unclear. There was already a thrombosis of the mesenteric vein but we noticed an extension and a worsening of the lesions leading to occlusive superior mesenteric vein at day 5, with a concomitant drop of the platelet count. This timing is the same as described in the literature, suggesting the hypothesis that the total occlusion of the superior mesenteric vein could be due to the addition of the two phenomena.

Diagnosis
The diagnosis of HITT relies on clinical evaluation as well as laboratory tests. The reference tests are two specific functional assays. There are several tools developed to assist the physicians with determining the probability of HIT. The most studied is the “4 T’s” score (Table 4).

This score is based on four clinical assessments: the degree of drop of platelet’s count, the timing of this decrease, thrombosis or other sequelae suspected and the presence of other possible causes explaining the thrombocytopenia. This score has a negative predictive value of 97% to 99% if this clinical pre-test score is low (0-3), allowing to rule out HITT. This tool is limited for intermediate or high score, regarding the poor specificity due to the high rate of false positives(20). When the score is intermediate or high, it is recommended to make further laboratory investigations. The first test to perform is enzyme-immunoassays for anti-PFA-4/heparin antibodies, which can highlight the presence of the immune response responsible for the platelet activation.
The sensitivity of this test is up to 99% but presents a lack of specificity because of detecting clinically insignificant antibodies (21). It is possible to optimize diagnostic accuracy by combining these immunoassays with a functional test of the platelets activation. These tests are much more specific for hit but they are restricted to specialized centres and should be used as second line tests (21) (Table 5 and 6).

Treatment
The key in management of HIT is the early cessation of the heparin. When clinical features are assessing an intermediate or high risk of HIT, the anticoagulation has to be promptly switched to a non-heparinoid treatment and immunoassays have to be done to confirm the diagnosis. The alternative therapy has to be focused on reducing the thrombin generation by using either direct thrombin inhibitors (argatroban, lepirudin or bivalirudin) or indirect factor Xa inhibitor (danaparoid, fondaparinux), but anticoagulation must not be stopped even in the absence of thrombosis. ACCP recommendations suggest that patients with HITT or HIT should rather be treated with argatroban, lepirudin or danaparoid than with vitamin K antagonists (VKA) (grade 1C) (18). VKA should not be prescribed until platelets have substantially recovered (grade 1C) (18) because it may exacerbate hypercoagulability due to faster depletion of protein C than prothrombin (19), leading to the recommendation that if VKA has already been started, vitamin K should be administrated (Grade 1C) (18). Seeing the drop of platelet count, it may be tempting to transfuse platelets. It should not be done for two reasons. The first is that spontaneous bleeding in hit is uncommon. Secondly, platelet transfusion increases the risk of thrombosis by increasing platelet activation because of the circulating antibodies. Platelets should only be given to patients who bleed or before invasive procedure with a high risk of bleeding (Grade 2C) (18). ACCP advocate to start VKA at low doses, when platelet count has reached 150 000/mm³ (Grade 1C). They also recommend to overlap VKA with non heparin anticoagulant for a minimum of 5 days and until the INR is within therapeutic range. There is no formal recommendation concerning the anticoagulation duration but ACCP suggests a 3 month period if HITT was noticed versus 4 weeks for an isolated HIT (18)
CONCLUSION
Pylephlebitis alone rarely leads to a total occlusion of the portal and mesenteric vein. If managed in time, most of them should resolve under an appropriate antibiotherapy and a therapeutic anticoagulation. Our case showed an uncommonly rapid and large extension of the portal thrombus to its tributaries leading to a vast ischemia of the small bowel. Regarding the literature, such complications were rare enough to make further investigations. Our analysis found two other prothrombotic conditions: heparin-induced thrombocytopenia type 2 and factor II G20210A mutation. Discussing HITT was important because it required modifying the anticoagulation treatment. This experience suggests that the extension of the thrombosis, while treatment is well guided, should raise concerns about other hypercoagulation factors. We incite physicians to rule out a prothrombotic predisposition for patients with unusual pylephlebitis. In the debate of anticoagulation for the management of pylephlebitis, our case focuses attention on a rare but devastating side effect of heparin: the HITT syndrome.
Clinical recommandations
- Start rapidly broad antibiotherapy and anticoagulation since the pylephlebitis is assessed
- Pay attention to drop in the platelet count between 4 to 14 days after introducing heparin
- If HIT is suspected use validated pre-test prior to further investigation; if score is at least intermediate switch directly heparin and initiate laboratory test to confirm the diagnosis
- If the lesions extend under well guided treatment, think to screen the patient for prothrombotic disorders or hypercoagulable state
Affiliations
1. MD Maccs en urologie
2. MD PHD, Service de chirurgie colorectale,
3. MD, Service de radiologie,
4. MD, Service d’hématologie
Cliniques universitaires Saint-Luc, B-1200 Bruxelles
Correspondance
Dr. Mehdi Bsilat
Urologie
Cliniques universitaires Saint-uc
Avenue Hippocrate 10
B-1200 Bruxelles
Références
- Loiseau D, Borie F, Agostini H, Millat B. [Sigmoid diverticulitis]. Gastroenterol Clin Biol 2005;29(8-9):809-16.
ouvrir dans Pubmed - Pradka SP, Trankiem CT, Ricotta JJ. Pylephlebitis and acute mesenteric ischemia in a young man with inherited thrombophilia and suspected foodborne illness. J Vasc Surg 2012;55(6):1769-72.
ouvrir dans Pubmed - Tang R, Tian X, Xie X, Yang Y. Intestinal Infarction Caused by Thrombophlebitis of the Portomesenteric Veins as a Complication of Acute Gangrenous Appendicitis After Appendectomy: A Case Report. Medicine (Baltimore) 2015;94(24):e1033.
ouvrir dans Pubmed - Bigsby E, Chaudhuri A, Whiteway A. Mesenteric and coeliac occlusions following heparin-induced thrombocytopenia after aortobiprofunda bypass surgery. Ann Royal Coll Surg Engl 2010;92(1):W15-7.
ouvrir dans Pubmed - Acosta S, Alhadad A, Svensson P, Ekberg O. Epidemiology, risk and prognostic factors in mesenteric venous thrombosis. B J Surg 2008;95(10):1245-51.
ouvrir dans Pubmed - Kanellopoulou T, Alexopoulou A, Theodossiades G, Koskinas J, Archimandritis AJ. Pylephlebitis: an overview of non-cirrhotic cases and factors related to outcome. Scand J Infect Dis 2010;42(11-12):804-11.
ouvrir dans Pubmed - Choudhry AJ, Baghdadi YM, Amr MA, Alzghari MJ, Jenkins DH, Zielinski MD. Pylephlebitis: a Review of 95 Cases. J Gastrointest Surg 2016;20(3):656-61.
ouvrir dans Pubmed - Sjobring U, Ringdahl U, Ruggeri ZM. Induction of platelet thrombi by bacteria and antibodies. Blood 2002;100(13):4470-7.
ouvrir dans Pubmed - Liappis AP, Roberts AD, Schwartz AM, Simon GL. Thrombosis and infection: a case of transient anti-cardiolipin antibody associated with pylephlebitis. Am J Med Sci 2003;325(6):365-8.
ouvrir dans Pubmed - Fukahori M, Shirayama S, Kawasaki A, Takasugi T, Sano H, Iwasaki H. A case of silent perforated diverticulitis in the ascending colon combined with pylephlebitis resulting in complete occlusion of the portal trunk. Clin J Gastroenterol 2015;8(4):172-8.
ouvrir dans Pubmed - Janssen HL, Meinardi JR, Vleggaar FP, van Uum SH, Haagsma EB, van Der Meer FJ, et al. Factor V Leiden mutation, prothrombin gene mutation, and deficiencies in coagulation inhibitors associated with Budd-Chiari syndrome and portal vein thrombosis: results of a case-control study. Blood 2000;96(7):2364-8.
ouvrir dans Pubmed - Chamouard P, Pencreach E, Maloisel F, Grunebaum L, Ardizzone JF, Meyer A, et al. Frequent factor II G20210A mutation in idiopathic portal vein thrombosis. Gastroenterol 1999;116(1):144-8.
ouvrir dans Pubmed - Plemmons RM, Dooley DP, Longfield RN. Septic thrombophlebitis of the portal vein (pylephlebitis): diagnosis and management in the modern era. Clinical infectious diseases : an official publication of the Infectious Diseases Society of America. 1995;21(5):1114-20.
ouvrir dans Pubmed - Baril N, Wren S, Radin R, Ralls P, Stain S. The role of anticoagulation in pylephlebitis. Am J Surg 1996;172(5):449-52; discussion 52-3.
ouvrir dans Pubmed - Allaix ME, Krane MK, Zoccali M, Umanskiy K, Hurst R, Fichera A. Postoperative portomesenteric venous thrombosis: lessons learned from 1,069 consecutive laparoscopic colorectal resections. World J Surg 2014;38(4):976-84.
ouvrir dans Pubmed - Greinacher A. Heparin-Induced Thrombocytopenia. N Engl J Med 2015; 373(19):1883-4.
ouvrir dans Pubmed - Krauel K, Weber C, Brandt S, Zahringer U, Mamat U, Greinacher A, et al. Platelet factor 4 binding to lipid A of Gram-negative bacteria exposes PF4/heparin-like epitopes. Blood 2012;120(16):3345-52.
ouvrir dans Pubmed - Linkins LA, Dans AL, Moores LK, Bona R, Davidson BL, Schulman S, et al. Treatment and prevention of heparin-induced thrombocytopenia: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest 2012;141(2 Suppl):e495S-530S.
ouvrir dans Pubmed - Hess CN, Becker RC, Alexander JH, Lopes RD. Antithrombotic therapy in heparin-induced thrombocytopenia: guidelines translated for the clinician. J Thromb Thrombol 2012; 34(4):552-61.
ouvrir dans Pubmed - Lo GK, Juhl D, Warkentin TE, Sigouin CS, Eichler P, Greinacher A. Evaluation of pretest clinical score (4 T’s) for the diagnosis of heparin-induced thrombocytopenia in two clinical settings. J Thromb Haemost 2006;4(4):759-65.
ouvrir dans Pubmed - Warkentin TE, Greinacher A, Gruel Y, Aster RH, Chong BH. Laboratory testing for heparin-induced thrombocytopenia: a conceptual framework and implications for diagnosis. J Thromb Haemost 2011;9(12):2498-500.
ouvrir dans Pubmed